Mpox: What you need to know about the latest public health emergency

But what is it, where did it come from and how the world might deal with this threat, it will certainly raise the specter of past pandemics like COVID-19 and the early spread of HIV infection?
Here’s what you need to know:

Mpox lesions commonly appear on the palms. (file)
What is Mpox?
Formerly known as monkeypox, this viral disease can spread between people, mainly through close contact and sometimes from the environment to people via objects and surfaces touched by people with monkeypox.
Originating in the Democratic Republic of Congo in 1970, mpox has been neglected there, according to WHO.
“It is time to take decisive action to prevent history from repeating itself,” speak Dimie Ogoina, host International Health Regulations Emergency Committeehas an advisory function to WHO on such matters.
The infection circulated in Central and West Africa, then caused a global outbreak in 2022, leading to a public health emergency by WHO in July when it became an outbreak in multiple countries.
After a series of consultations with global experts, WHO has begun using the newly preferred term “mpox” as a synonym for monkeypox. Learn more about that decision This.
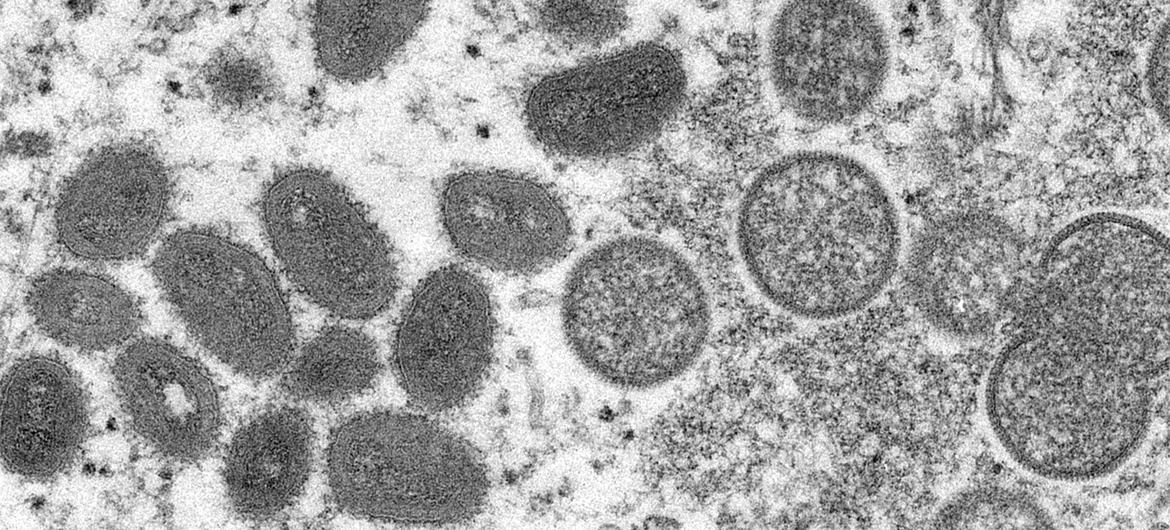
Mpox is similar to the smallpox virus that has been eradicated. (file)
What are the symptoms?
Common symptoms of mpox include a rash that lasts two to four weeks, which may begin with or be followed by fever, headache, muscle aches, back pain, fatigue, and swollen lymph nodes.
The rash looks like blisters and can affect the face, palms of the hands, soles of the feet, groin, genital and/or anal areas, mouth, throat, or eyes. The number of sores can range from one to thousands.
People with mpox are considered to be at least contagious until all their blisters have crusted over, the scabs have fallen off and new skin has formed underneath, and all lesions in the eyes and throughout the body have healed. This usually takes two to four weeks. There are reports that people can become reinfected after they have had mpox.
People with severe MPOX disease may require hospitalization, supportive care, and antiviral medications to reduce the severity of damage and shorten recovery time.
How is mpox disease spread?
From person to person: WHO said touching, having sex, talking or breathing close to someone with mpox could generate potentially infectious respiratory particles, but more research is needed into how the virus spreads during outbreaks in different settings and conditions.
What scientists do know is that the virus can also survive for a while on clothing, bedding, towels, objects, electronics, and surfaces that an infected person touches. Other people who come into contact with these objects can become infected without washing their hands before touching their eyes, nose, and mouth.
The virus can also be spread during pregnancy to the fetus, during or after birth through skin-to-skin contact, or from an infected parent to a newborn or young child during close contact.
Although there have been reports of mpox infection from asymptomatic people, there is limited information about whether the virus can be transmitted from people who are infected before they have symptoms or after their lesions have healed.
From human to animal: Because many animal species are susceptible to the virus, it is possible that the virus can spread from humans to animals in different settings.
People with confirmed or suspected mpox should avoid close contact with animals, including pets such as cats, dogs, hamsters, and gerbils, as well as livestock and wild animals.
From animals to humans: A person who comes into physical contact with an animal that carries the virus, such as certain species of monkeys — or a terrestrial rodent like a tree squirrel — can also get mpox. Such contact can occur through a bite or scratch, or during activities such as hunting, skinning, trapping, or preparing food. The virus can also be contracted through eating infected meat that is not thoroughly cooked.

A health worker checks on a two-year-old boy being treated for mpox in northern Goma, Democratic Republic of Congo.
Can it be fatal?
Yes, for a small minority. Between 0.1 percent and 10 percent of people infected with mpox die.
According to the UN health agency, it is important to note that mortality rates in different settings can vary due to a number of factors, such as access to health care and underlying immunodeficiency, including due to undiagnosed or advanced HIV.
In most cases, symptoms of mpox will clear up within a few weeks with supportive care, such as pain or fever medications, but in some people, the disease can become severe or lead to complications and death.
Infants, children, pregnant women, and people with underlying immunocompromising conditions — such as advanced HIV infection — may be at higher risk of more severe mpox disease and death.
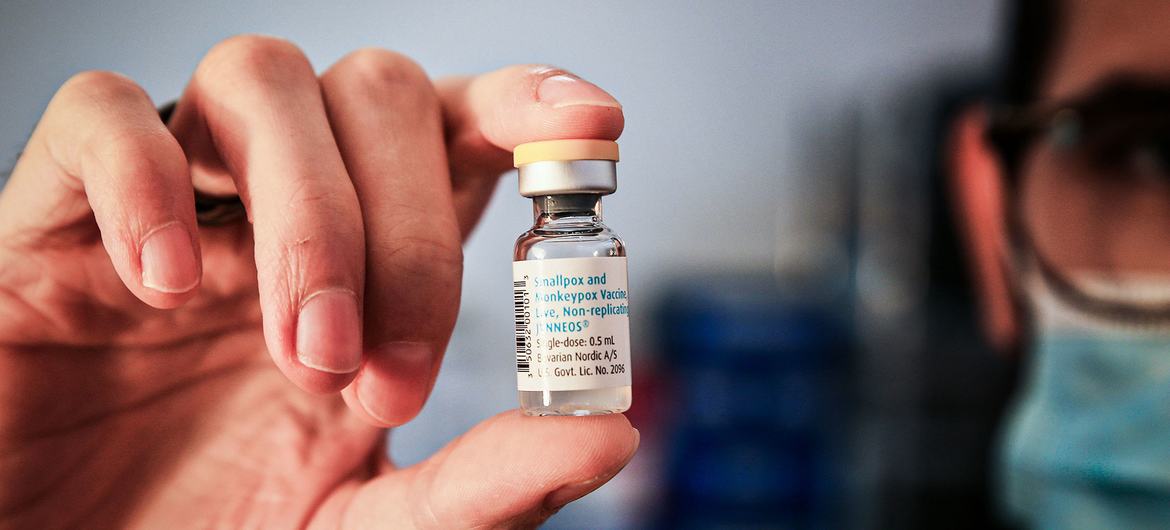
A single dose of mpox vaccine.
Is there a vaccine?
Yes. The United Nations health agency recommends several vaccines to protect against mpox. However, mass vaccination, which is being rolled out during the global COVID-19 pandemic, is not currently recommended.
Years of research have led to the development of newer, safer vaccines for the now-eradicated smallpox disease. Some of these vaccines have been approved in many countries for use against smallpox.
Currently, WHO recommends the use of MVA-BN or LC16 vaccines or ACAM2000 vaccines when other vaccines are not available.
According to the WHO, only people at risk of exposure to mpox should be considered for vaccination. Travelers who may be at risk based on an individual risk assessment with their healthcare provider may want to consider vaccination.

One way to prevent the spread of mpox is to wash your hands after touching contaminated surfaces.
How to prevent mpox disease?
Cleaning and disinfecting surfaces or objects and washing hands after touching surfaces or objects that may be contaminated can help prevent transmission.
The risk of getting mpox from animals can be reduced by avoiding unsafe contact with wild animals, especially sick or dead animals, including their meat and blood.
In countries where animals carry the virus, any food containing meat or animal parts must be thoroughly cooked before eating.
Learn more about mpox This.


